Definition
Is a multifactorial disorder caused by diminished insulin action due to its decreased availability or effectiveness in varying combinations.
Types of diabetes:
(based on aetiology)
Type 1: immune mediated or idiopathic
Type 2: insulin resistance /insulin deficiency
Type 3:
- · genetic syndromes
- · drug induced
- · hormonal
- · malnutrition related etc.
Type 4: gestational diabetes
Diagnosis
With symptoms:
A random blood sugar of >11.1mmol/l (200mg/dl) is diagnostic
Without symptoms:
· WHO (1985)
FBS 2hr PGBS
= or> 7.8mmol/l and/or =or>11.1 mmol/
(140mg/dl) (200mg/dl)
(IGT :FBS <7.8 and PGBS 7.8-11.1)
· ADA (1997)
FBS= or> 7mmol/l
(126mg/dl)
(IFG: 6.1 - 6.9 mmol/l)
WHO (1999)
FBS = or>7mmol/l
(IGT:7-11.1mol/l)
Presentations:
(1) Routine examination
(2) Clinical symptoms:
· Thirst Pruritus vulvae
· Polyuria Balanitis
· Polydipsia Impotence
· Nocturia Changes in vision
· Wt. Loss Parasthesiae
· Tiredness
(3) Ketoacidosis
(4) Symptoms of complications
a) Nephropathy Nodular glomerulo sclerosis
(Kimmelsteil Wilson ) NS
CRF
Proteinuria
Gen. Arteriosclerosis
Pyelonephritis
Symptoms of anaemia
Uraemia
N.S.
b) Retinopathy
I. Simple or background microaneurysms
Blot.hges
Exudates
Cotton wool
Tortuous veins
2. Proliferative retinopathy neovascularization
vitreous haemorrhages
3. Exudative retinopathy macular oedema
macular exudates
Cataract – snow flake in Type I
Accltd. Senile in Type 2
c) Macroangiopathy:
Atheroma in large and medium sized blood vessles
CVD
IHD
PVD
c) Macroangiopathy:
Atheroma in large and medium sized blood vessles
CVD
IHD
PVD
d) Neuropathy:
a. Peripheral neuropathy:
Sensory
Motomotor
? mixed
(Charkot’s neuroarthropathy)
b. Aut. Neuropathy, post. Hypotension
Impotence
Bladder retention
Bowel diarrhoea
Gust sweating
c. Mononeuropathy CTS
Lat.pop
Cervical sp.root
TI
e. Dermopathy: Carbuncles
ulcers
muco cutaneous candidiasis
EVALUATION OF A DIABETIC PATIENT
First visit
History
• History
• SYMPTOMS OF DIABETES
polyuria, nocturia, polydipsia polyphagia, recent weight loss or weight gain, tingling, numbness or pain in the hands and or feet (night cramps), pruritus, vaginal discharge, balanitis.
• DIABETIC HISTORY
Age at which diabetes was detected, duration of disease, family history, previous and current treatment
Drug history (steroids)
• PAST HISTORY
HT, Hyperlipidaemia, IHD, stroke, PVD, liver disease,erectile dysfunction.
Smoking, alcohol history, 24 hour dietary recall
EXAMINATION
Anthropometric measures
- Height
- Weight
- Body mass index- Weight in kg / (Height in m)2
- Waist circumference
Detailed examination
- Including signs of insulin resistance like acanthosis nigricans, skin tags
- Signs of Hyperlipidaemia e.g.: xanthelasma, xanthomas.
- Pay particular attention to cardiovascular system, check blood pressure
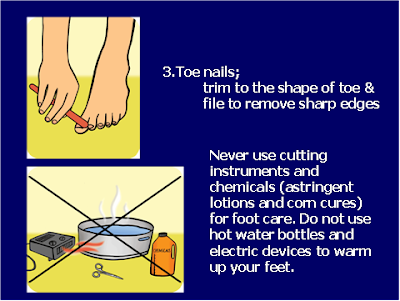
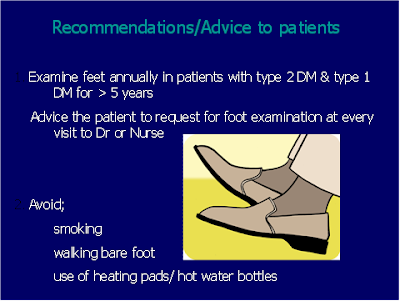
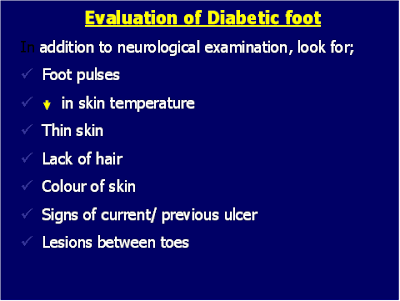
• Foot examination
- a must in every diabetic patient – skin, nails, hair, temp, pulses.
• Dilated fundoscopy
EVALUATION OF A DIABETIC PATIENT
First visit
• What type?
• Are there complications?
• Any underlying cause?
• Risk factors of CAD?
Features of Type 1 diabetes
• Early onset
• Children/young adults
• Generally thin
• Not responding to OHAs
• C-peptides
Features of Type 2 diabetes
• Family history present
• Obese or nonobese
• Middle aged or elderly
• Features of metabolic syndrome
Visceral Fat
Features of Type 3 diabetes
· Iatrogenic
· Endocrine
· Malnutrition
· Pancreatic Diabetes
· Genetic syndromes
Are there complications
· Retinopathy
· Nephropathy
· IHD
· CVD
· PVD
· Skin
· Foot
Nephropathy
· Hypertension
· Proteinuria
· Retinopathy
Ischaemic heart disease
· History
· Hypertension
· Peripheral pulses
· Carotid bruits
· ECG
· Xanthomas
Cerebrovascular disease
· History
· Carotid bruits
Peripheral Vascular Disease
· Peripheral pulses
· Vasomotor changes
· Ulcers
Skin
· Dermopathy
· Ulcers
· Cellulitis
· Necrobiosis diabeticorum
· Mycoses
· Gangrene
Foot
· Curvatures
· Deformities
· Ulceration
· Callosities
· Fissuring
Investigations
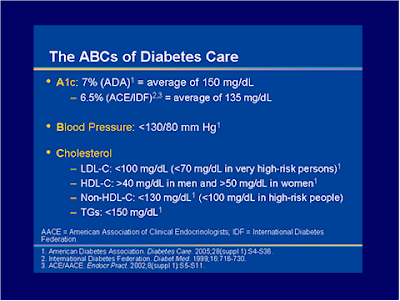
– FBS and PPBS
– HbA1C
– Fasting lipid profile
– Blood urea and electrolytes
– Urine analysis: Ketones, protein, glucose
– Urine Microalbumin-
– ALT, AST, ALP
– ECG
– Islet cell antibody/GAD antibody if considering type 1 diabetes
Treatment
To allow the patient to lead a comfortable normal life and to prevent complications
3 methods of treatment:
1. Diet alone 60%
2. Diet and oral hypo. Agts. 20%
3. Diet and insulin 20%
Choice of therapeutic regimes
1. Type I <40 most will need insulin
2. >40 specially obese ones could be controlled on diet alone
3. >40 who fail with diet.
§ Non obese: sulphonylureas
§ Obese: biguanides
Failure: may need insulin
Diet Principles:
a. Total cal. Requirement age, sex, occupation
Actual weight in relation to ideal weight
Economic status
b. Proportion of cals from CHO 60 (instd.of 46%)
Prts 15 (……….. 12%)
Fats 25 (………. 42%)
c. Local availability and preference
d. Foods well spread through out the day
e. Foods should be of high fibre content (slowly digested and absorped)
Oral hypoglycaemic agents
a. Sulphonylureas act by sensitising beta cell to the action of glucose
increase insulin receptors.
Eg. Chlorpropamide
Tolbutamide
Glibenclamide
Glipizide
b. Biguanides . act by reducing hepatic gluconeogenesis
Increasing peripheral utilisation of glucose
Useful in obese diabetics
Danger of lactic acidosis with phenformin
C.Others:repaglinide,acarbose,troglitazone
Oral hypoglycaemic agents
a. Sulphonylureas act by sensitising beta cell to the action of glucose
increase insulin receptors.
Eg.
· Chlorpropamide
· Tolbutamide
· Glibenclamide
· Glipizide
b. Biguanides . act by reducing hepatic gluconeogenesis
Increasing peripheral utilisation of glucose
Useful in obese diabetics
Danger of lactic acidosis with phenformin
C.Others:repaglinide,acarbose,troglitazone
Insulins
Indications:
a. Type I diabetes
b. Type 2 where maximum doses of OHA have failed(sec.OHA failure)-
c. Type 2 younger patients to prevent tissue damage
d. With complications (specially young pts)
Infections
Ketoacidosis
Neuropathy
Foot lesions
e. pregancy
f. glucose toxicity
Types of insulins
Species: purity: Duration:
Bovine conventional Short
Porcine single peak intermediate
Human highly purified long
Rapid-Acting Insulin
• Lispro (Humalog)
• Insulin Aspart (Novorapid)
• These are used as bolus (mealtime) insulin
Short-Acting Insulin
• Regular insulin (Actrapid /Humlin R)
• Short-acting
• Onset of action 30-60 minutes
• Duration of action 5-8 hours.
• To be taken 20-30 minutes before meals.
Intermediate-Acting Insulin
• NPH (Insulatard/ Humulin N) & Lente
• Their appearance is cloudy
• Onset of action is about 2 hours after injection
• Peak effect is from 6-10 hours
Long-Acting Insulin
• Detemir (Levemir)
• Glargine (Lantus)
– peakless delivery over 24 hours.
– Clear in solution
– Cannot be mixed with other insulin
– Usually given at bedtime.
– Lower fasting glucose levels and less hypoglycemia
Pre-Mixed Insulin
• 70/30 means 70% NPH and 30% Regular
• 50/50 means 50% NPH and 50% regular
• Addition of protamine to lispro: used in 75/25 combinations
• Protamine to aspart: 70/30 combination (Novomix 30)
Administration:
1. Low dose frequent
2. Sliding scale
3. According to previous blood sugar estimation
Comas in diabetes
1. Hyperglycaemic : Keto acidotic
Non keto acidotic
2. Hypoglycaemic
3. Other metabolic comas:
sec. to diabetes uraemia
Lactic acidosis
4. Other independent causes ex. SAH
Ketoacidosis
Pathogenesis: Pptd by infections
Trauma
Drugs
Non compliance
Clinical: Air hunger Anorexia
Dehydration vomiting
Ketone smell Abd. Pain
Wt loss Low BP
Fatigue
Non ketotic. Usually in elderly
Only dehydration is present
Investigations:
Blood sugar HCO3
Urea PCV
Na, K UFR
pH ECG
Hb
Treatment:
a) Fluids, N. Saline
I lit. first 1/2 hr
I lit next hour
I lit next 2 hrs
Then 500 ml hrly total of 5l.Change to 5% dext. when blood sugar is 10-16 mmol.alternating with N saline
b)Insulin: Sol. Insulin 20 units IV
10 units IM hrly till blood sugar is 13mmol.
Then 10 units SC 4 hrly
c)Potassium: add I.gm(20mmol) to each L of fluid Beginning with second L of N saline
Omit K if S.K is over 6 mmol.
d) HCO3, 100mmol of NaHCO3 if pH is below 7.1 Ppt. In 1 to 1 1/2 hrs if pH is still less than 7.1
e) Gen. Management:
Monitor pulse, BP, CVP urine output.
NG suction
Oxygen
Catheterise bladder
Monitor blood sugar, electrolytes, urea, pH
HCO3 4 hrly
Ppting treat , cause
Mangement of unconcious state
DIC
Hypoglycaemia
Hypo Hyper
by inc. insulin Infection
starvation stress
Exercise Non compliance
Onset: sudden gradual
Clinical:
Drowsy Drowsy
Pupils dilated Normal size
Bounding pulse Low vol. Pulse
BP n. or inc. sys Normal or low
Hydration normal Dehydarated
Breathing normal acidotic
Urine output normal reduced
Fits fits unusual
Abn. Behavior Abn. Behaviour unusual
Lab, Low BS, pH, HCO3, BU














Tidak ada komentar:
Posting Komentar